When we talk about smoking cigarettes, we usually discuss the harmful effects that it has on our lungs, mouth, skin, and other parts of the body. However, we don't often talk about the gut even though cigarette smoke is the best-known environmental risk factor for Inflammatory bowel diseases (IBD), Crohn’s disease and ulcerative colitis. While the exact mechanism for why people get these diseases is not yet known, it is recognized that a dysbiosis of the gut plays a contributing role to the onset of these conditions. A research team in Germany investigated the effects that cigarette smoke exposure had on the mucus layer and the microbes in the gut.
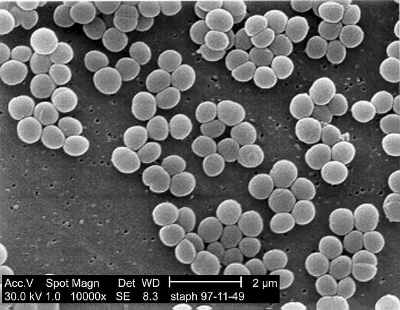
The scientists exposed mice to cigarette smoke or air for a period of 24 weeks. They found there was a shift in the microbial community in the caecum and distal colon after exposure to smoke. Specifically, there was an increase in Lachnospiraceae in the colon however it remained the same in the ileum, the last part of the small intestine.
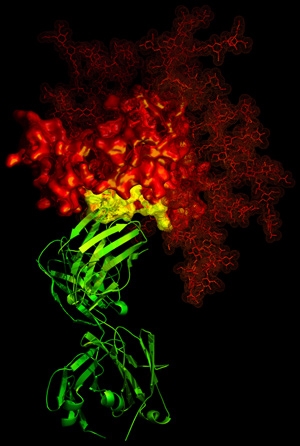
They also found that smoke exposure led to changes in mucin exposure. Mucin is a type of protein that is known for producing gels that act to lubricate and protect parts of the body, both internal and external. The most common mucins are Muc2, Muc3, and Muc4. Muc2 for example is a protein that is secreted onto the mucosal surfaces of the large intestine and serves as a protective barrier for the epithelium. In this study, they found that Muc2, Muc3, and Muc4 gene expression was altered after cigarette smoke exposure.
The authors hypothesize that cigarette smoke affects the immune system in the ileum and may lead to the inflammation associated with Crohn’s disease. Overall, this study found that exposure to cigarette smoke had a profound effect on the gut bacteria and mucin composition in the mouse. While this was not done in humans, the same effects would likely be seen.