The Tara, the boat used for this 3.5 year journey
photograph by Yohann Cordelle distributed under a CC-BY 3.0 license
Today’s blog diverges a bit from our normal topics yet it may have important implications to understanding the microbiome of the human body. Like the human body, the ocean is made up of microbes that interact with one another and play a critical role in shaping the ocean’s ecosystem, just on a slightly larger scale. To map out the microbial communities, and specifically plankton, of the world’s oceans, an international team of microbiologists, scientists, and others set out on a three and a half year journey aboard the ship Tara.
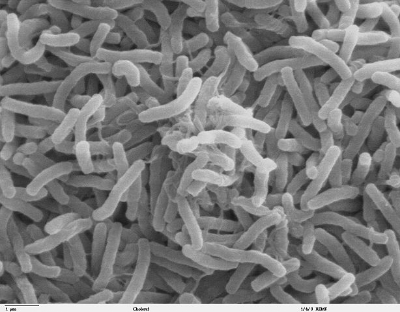
The Tara Oceans Consortium resulted in five papers published recently in Science. The scientists traveled around the world and collected 579 samples from 210 locations in every major oceanic region. They sampled at any given site for about 60 hours using standardized protocols to ensure they were accurately capturing the genetic diversity of the plankton in any given region. Plankton are mostly invisible to the naked eye and largely uncharacterized, yet they are an essential to the ocean’s food web and also produce approximately half of the world’s oxygen.
One of the five papers describes a catalog of the genetic samples found in the study called The Ocean Microbial Reference Gene Catalogue. This catalog contains 40 million genes, four times the number in the human gut microbial gene catalog, from over 35,000 plankton species. In comparison to the human gut, despite their differences, such as the gut lacking oxygen and having a stable temperature, there was a significant overlap between the two microbiomes. This led the investigators to hypothesize that it may be possible that microbiomes despite their ecosystem function in largely the same way.
The new microbial ocean catalog contains genes from mostly prokaryotic, or uni-cellular, organisms. Over 81% of the genes explored in the Tara Oceans expedition were unique to this study and did not match any previous reference genomes. This striking number highlights the fact that despite great investigation into the ocean, the ocean is still largely unknown and unexplored. The deeper the scientists went into the ocean, the novelty of the genes identified also increased. Temperature was also an important factor into the diversity of samples collected as changes in ocean temperature was the most important environmental factor that drove community composition.
This project has laid the groundwork for greater analysis of the oceans’ plankton and microbial communities and will improve models of the ocean. For example, the finding that temperature was the key driver for microbial community variation could have important implications for better understanding climate change. The information collected aboard the Tara not only helps us better understand the ocean’s microbiome but it allows scientists to compare across ecosystems and better understand microbial communities in general.