Past studies have shown an association between hormonal contraceptives and risk of HIV-1 infection, as well as between genital tract infection and acquisition of HIV-1. The types of hormonal contraceptives that have been associated with increased risk of HIV include progestin injectable depot medroxyprogesterone acetate (DMPA) and combined estrogen-progestin oral contraceptives (COC). Untreated cervical pathogens such as Trichomonas vaginalis, Neisseria gonorrhoeae, Chlyamydia trachomatis, Candida albicans, and genital herpesvirus 2 also contribute to increased risk of HIV. In a study recently published in mBio by the American Society for Microbiology, researchers investigated the combined effects of hormonal contraceptives and genital tract infections on risk level of HIV.
The participants of this study were 633 HIV-negative women and 199 HIV-positive women, all of whom live in Uganda or Zimbabwe. It was found that more than half the study participants were positive for herpes. Cases of herpes were evenly distributed among women with chlamydia, candidiasis, and bacterial vaginosis. However, herpes was significantly more common among women positive for T. vaginalis or gonorrhea. As for contraceptives, women with asymptomatic infections were mainly COC users (65%) followed by DMPA users (60%). Symptomatic infections were most common in the group that did not use hormonal contraceptives.
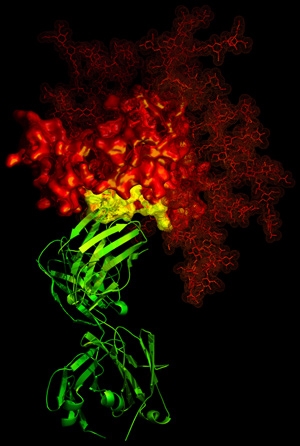
To test for risk factors of HIV, the researchers looked at certain immune system response components. It was found that HIV was associated with higher levels of two immune components known as RANTES and BD2. RANTES was seen to be increased among combined estrogen-progestin oral contraceptive users whom were also associated with herpes and abnormal vaginal microbiota. BD2 was seen increased among COC and non-HC users by T. vaginalis infection and among DMPA users by herpes, candidiasis, and bacterial vaginosis.
As is common in all processes of life, there seem to be many factors that contribute to HIV infection. Changes in the immune system caused by hormones, like contraceptive hormones, and genital bacteria composition may combine to influence vulnerability to HIV infection. This study is important, because the more knowledge scientists have about women’s reproductive health, the greater the possibility that we can develop treatment and prevention plans for infections.