In 2013 there was an avian flu (H7N9) outbreak in China that affected 140 people, killing 46 of them. During the outbreak doctors from one of the major hospitals in China treated 40 of these patients by giving them antivirals and antibiotics, amongst other first line treatments. In addition, they gave probiotics along with the antibiotics to restore the gut microbiome. All the while, they measured the patients’ microbiomes to track how they changed throughout the course of treatment. The results of this study were published last week in the journal Nature Scientific Reports.
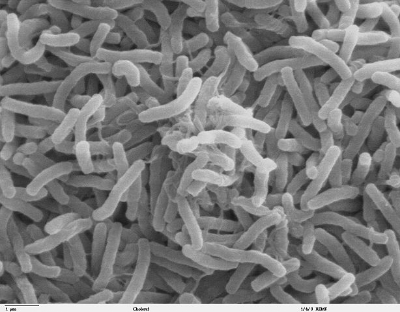
Twenty six patients were enrolled in the study, and each of them was given antibiotics within 6 hours of admission to the hospital. In addition, each one was given Clostridia probiotic capsules along with the antibiotics. Thirty one healthy control stool samples that represented the demographics of those undergoing flu treatment were also measured as a part of the study. Before the antibiotics were taken, the patients with the flu already had altered microbiomes that were low in diversity and had lower abundances of Bacteroidetes and higher levels of Proteobacteria. After antibiotics were given there was a dramatic shift in the microbiomes, that was characterized by a relative increase in the abundance of Escherichia coli. In addition, the scientists noted that the probiotics were in fact increasing the amounts of Clostridia in the guts of patients who took them, and that the probiotics may have led to better clinical outcomes. In their hospital only 20% of patients died of the flu, whereas 40% died in the rest of China.
The major takeaway from this study is the changes that the flu has on the microbiome, decreasing diversity and altering the levels of certain phyla. The fact that the probiotics did appear to take hold and improve clinical outcomes is interesting, but the study was extremely small and limited in its scope to reach any statistically significant conclusions. Overall though, this study suggests that if you come down with a flu that it may be wise to feed and nourish your microbiome because it is ‘getting sick’ right alongside you.