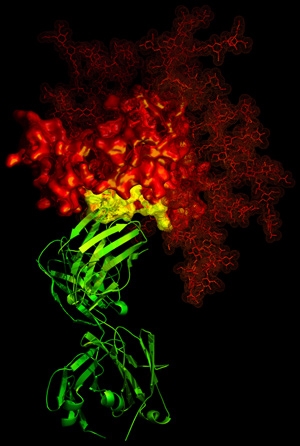
Scanning electron micrograph of HIV-1, colored green, on a lymphocyte.
From 2009 to 2013, scientists at Duke University and the National Institute of Allergy and Infectious Diseases had been working on what looked like a promising cure to HIV. The study was terminated in 2013 because it was clear that the vaccine was not effective in protecting against HIV infection. An article recently published by Science Magazine gave insight into why the HIV vaccine unfortunately failed. Hint: it has something to do with the microbiome.
The vaccine was administered in the study to adult males in the form of an initial vaccine as well as a second booster vaccine. The HIV vaccine looked promising because it stimulated the body’s immune system to produce antibodies that recognize HIV. The unexpected result, however, was that these antibodies also recognized bacteria like Escherichia coli, a very important bacteria that lives in the human gut. It should be easy to see why this is a bad thing for the microbiome. Destroying important gut bacteria is very detrimental to humans, which we see over and over again here on the blog. Additionally, because the antibodies were reactive to bacteria as well as the HIV virus, it took away from the effectiveness of fighting HIV.
This study is very important in the search towards finding a cure to HIV, because it presented an unexpected obstacle that a lot can be learned from. Moving forward, questions are already being raised by the scientists such as, would this vaccine work for children if immunization was given to pregnant mothers? Perhaps the still-developing immune system would better be able to work with the vaccine. Only more research can prove whether the HIV vaccine is indeed still promising. In addition, this may provide insights into the efficacy of vaccines for other diseases. Perhaps the microbiome plays a large role in their effectiveness. Vaccine research going forward should begin to take the microbiome into account.