There are many diets that have been rigorously shown to decrease metabolic syndrome (obesity, diabetes, etc.) and are generally associated with a healthy lifestyle, such as vegetarian, vegan, and Mediterranean diets. The one thing they share in common is a high consumption of plant material, and a low consumption of meat. There are mechanistic reasons for why high veggie - low fat diets should improve health, and many researchers now believe this is partly due to the gut microbiome that these diets create. In order to help demonstrate the microbiome-mediated health benefits of a high vegetable – low meat diet, a team of researchers from Italy recently measured the microbiome and specific metabolites produced by the microbiome in 153 individuals. They then compared these results with the diet that the individual had consumed prior to the measurements, and confirmed that these ‘healthy’ diets were creating ‘healthy’ microbiomes. They published their results in the journal Gut.
The scientists asked 51 vegans, 51 vegetarians, and 51 ominivores individuals to self-declare their eating habits over the past seven days, and then sampled their stool and urine for bacteria and metabolites. They learned that amongst the different types of diet the individuals’ overall microbiome diversities were relatively similar. However, they did show that Bacteroidetes were more prevalent in vegetarians and vegans than in ominvores, and that a higher Firmicutes to Bacteroidetes ratio existed in the guts of ominvores than in vegans and vegetarians. In addition, the abundance of Prevotella, which is normally associated with health, was positively correlated with overall vegetable intake, and on the contrary Ruminococcus was negatively associated with a high vegetable diet.
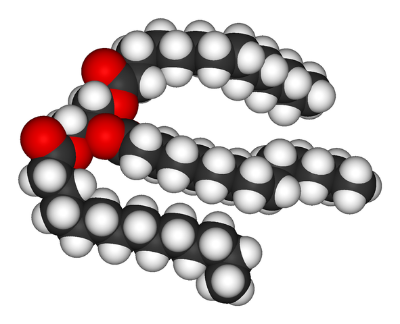
The scientists also measured specific metabolites in the individuals. They discovered that short chained fatty acids (SCFAs), which are normally implicated with health, were associated with the consumption of fruits, vegetables, and legumes. In addition, there were positive associations between SCFAs and specific populations of bacteria, such as Prevotella. On the other hand, the metabolite trimethylamine oxide (TMAO), which is a microbiome metabolite whose concentration is directly related to atherosclerosis and other diseases, was significantly lower in vegetarian and vegan diets compared to omnivore diets. It was also directly associated with the abundance of the aforementioned Ruminococcus.
These relationships between SCFAs and veggies are unsurprising, because SCFAs are the byproducts of bacteria breaking down the complex glycans found in fiber. In addition, the TMAO is produced by gut bacteria from carnitine and choline, two molecules that exist in red meat and eggs, among other things. Regardless though, this study should remind us that our diet can shape our microbiome and have lasting health effects. This study only reinforces that a diet high in veggies that feeds the microbiome is probably a healthy choice.