As we read on yesterday's blog post, dietary fibers alter the microbiome. On this week's episode of The Microbiome Podcast we talked in depth with Drs. Erica and Justin Sonnenburg from Stanford University about dietary fibers and their impact on our microbiota and our health. Erica and Justin wrote a book that was published today called The Good Gut: Taking Control of Your Weight, Your Mood, and Your Long-term Health. You can buy it here on Amazon and it's a highly recommended read for anyone interested in the microbiome.
Check out the newest episode on iTunes, Stitcher, or listen on our website.
We will continue answering your questions on the podcast so please call 518-945-8583 with any questions for us or for next week's guest, Dr. Elaine Hsiao.
See below for more detailed show notes from today's episode:
(1:17) Dr. Rob Knight received a Creative Promise in Biomedical Science Prize from the Vilcek Foundation. Read more.
(3:09) Rob Knight also published a book called Follow Your Gut: The Enormous Impact of Tiny Microbes. Click here to buy it on Amazon.
(3:33) uBiome recently began a pregnancy microbiome study to better understand how the bacteria in our bodies change during and after pregnancy. Find out more on the uBiome website.
(4:56) Microbiome Therapeutics performed a clinical study with an investigational drug in type 2 diabetics taking metformin and found that the drug resulted in more tolerability for patients and fewer side effects than metformin without the drug. Read more.
In the (9:40) conversation with Erica and Justin Sonnenburg (read more about their research), we talked about several topics pertaining to diet and dietary fiber and its impact on our microbiota and health. We also discussed:
(11:49) Why they decided to write the book.
(16:05) Their personal experiences having children and the importance of nurturing their health and its impact on their lives.
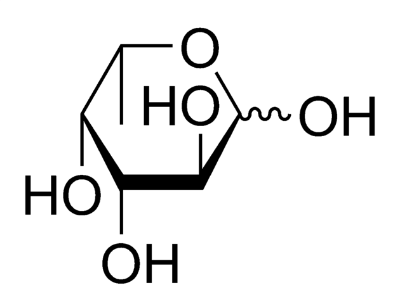
(17:55) Dietary fibers and differences among various types of fibers in our diets.
(26:15) How fast does diet change the microbiota?
(32:05) Bacteroides thetaiotaomicron and why it is Erica and Justin's favorite microbe and a study Justin published in 2005 while he was in Jeff Gordon's lab. Read the paper here.
(37:35) How microbiome therapies are going to look in the future.
(41:00) How eating better can make an impact now on our overall health. Read the seminal obesity and microbiome paper Erica mentions from the Gordon laboratory.
We also answered two other (44:00) listener questions about phage therapy and organic vs. non-organic baby and adult foods.
Next week we will be talking with Dr. Elaine Hsiao from Cal Tech so please call 518-945-8583 with your questions about autism and the microbiome as well as the microbiome's ability to regulate serotonin levels.