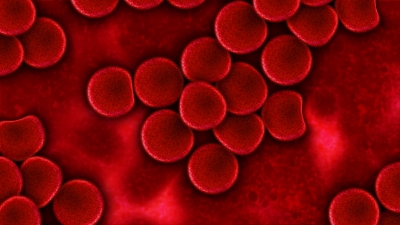
Candida albicans growing in petri dish
Celiac disease is a serious autoimmune disorder in which gluten, found in wheat, rye, and barley, triggers an immune response that damages the absorption capabilities of the intestines. The AMI has covered this topic in a few previous blogs (click celiac disease tag below) in relation to autoimmune disorders and possible bacterial triggers. One contributing factor to the celiac disease response is due to the protein gliadin, which is found in gluten. Gliadin, along with transglutaminase (which is a human protein that binds to, and deaminates gliadin), trigger a T Cell response that leads to the inflammation and tissue damage.
The yeast Candida albicans is a common gut commensal that is linked to inflammatory bowel diseases and vaginal infections. This yeast also binds with transglutaminase, using a protein called Hwp1, in an identical fashion as gliadin. This results in the bacteria’s strong binding to the intestinal wall, where it triggers an autoimmune response to destroy the yeast.
Researchers in France hypothesized that the similarity between gliadin's and C. albicans' binding to transglutaminase may result in a similarity in the body's response to these two things. In essence, they suggested that gluten ‘tricks’ the body into an immune response because it 'looks' similar to C. albicans.
In the study, recently published by Plos One, blood cultures from 87 adult patients with celiac disease and 41 patients with C. albicans infection were collected. The scientists then isolated the body's natural antibody for Hwp1 and measured its response to both gliadin and Hwp1. They discovered that gliadin also binds to Hwp1's antibody, meaning that it should elicit the same immune response as Hwp1. Therefore, the body should mount an immune response for gluten that is characteristic of C. albicans infection, and this response could manifest itself as celiac disease.
The significance of this study is that it comes closer to finding a cause and prevention of celiac disease. The T cell immune response that results from transglutaminase binding to gliadin could initially be triggered by a C. albicans yeast infection. This may explain why some people only become gluten sensitive later in life - perhaps it only occurs after they have a C. albicans infection and the body builds up antibodies for this yeast. This is another example of how microbes found in healthy individuals can be harmful when homeostasis is not controlled.