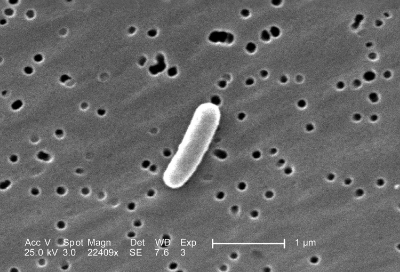
Scanning electron micrograph of E. Coli bacterium.
Curtis Huttenhower, Rob Knight, Owen White, Jacques Ravel (all members of our SAB), and others recently published a commentary titled "Advancing the Microbiome Research Community" in Cell. The paper was a 'State of the Microbiome' address and outlined the current challenges and the future outlooks of the microbiome field.
Among the many challenges they outlined include how to design causality studies, and how to attribute causality of phenotypes to specific bacteria, proteins, or metabolites. The paper also discussed the bioinformatics bottleneck that is occurring in the field, as the necessary expertise required to properly analyze sequencing data is severely lacking. There also lacks a proper centralized online repository for all sequencing data that is generated. This sequencing data needs to include metadata that would describe how the data was generated. Furthermore, the authors describe the need for guidance on how to properly define and comprehensively describe phenotypes, such as inflammatory bowel disease (IBD), in microbiome studies. Without this standardization, proper comparison between studies can not take place. Finally, institutional review boards (IRBs) need guidance on how to properly regulate human microbiome studies in order for scientists to properly prepare and carry out their projects.
While the above areas are only a few of the challenges facing the field, each of them reinforces the mission and programs of the AMI. The MBQC is standardizing techniques and creating rigorously tested analytical protocols by investigating the sources of variation in microbiome testing. In addition, the AMI is focusing on future data repository efforts. These are just a few of the areas we hope to serve the field in the coming years. We believe a nonprofit, specifically the AMI, can help fill these voids and address many of the issues outlined in this paper.