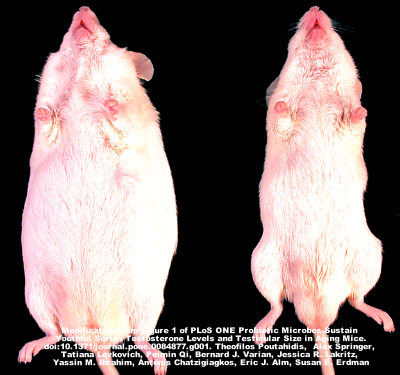
iChip - the device used to identify the new antibiotic (image by Slava Epstein/Northeastern University)
Antibiotic resistance is a topic that we’ve written about extensively in the blog and a major public health concern in today’s society. In the US alone, over 20,000 deaths are caused by antibiotic resistant bacteria every year and several million illnesses can also be attributed annually to antibiotic resistant bacteria. Research led by Dr. Kim Lewis at Northeastern University resulted in the identification of a new antibiotic called teixobactin that looks as if it may not cause antibiotic resistanace. This discovery is being hailed as groundbreaking and a promising avenue to treat previously untreatable chronic infections.
The research published on Wednesday in Nature identified this new antibiotic by culturing bacteria that were previously difficult to grow in the laboratory. Only about 1% of microbes can be grown in the laboratory making the identification of new antibiotics very difficult (antibiotics are generally developed using microbes). Using a device called the iChip, they were able to successfully grow up to 50% of bacteria that were previously unable to be grown in the lab.
Cells from different bacterium were placed individually into a chamber on the iChip that holds several hundred chambers. The device is then placed under the soil where the bacteria are able to grow in their natural environment. After they form colonies, the device was brought to the laboratory and the bacterial colonies were placed on a petri dish. A target bacteria is then covered over the bacteria that were growing in the soil. If they see that there is no growth over a specific area, they know that the bacteria in that chamber is releasing a potential antibiotic. Through this method, the scientists identified 25 promising novel antibiotics in which teixobactin was the most promising.
Two diseases we’ve discussed on the blog previously are MRSA (methicillin resistant Staphylococcus aureus) and Clostridium difficile infection. C. diff is a disease usually caused when the healthy bacteria in the gut are killed by an antibiotic and C. diff colonizes the gut. This can be very difficult to treat and a last resort is often a fecal microbiota transplant (FMT). An exciting development from this research is that this new antibiotic was particularly effective against both C. diff and S. aureus as well as the bacteria that causes tuberculosis.
This is an incredibly exciting development but as an organization focused on the microbiome, we need to think about what the implications are on the microbiome. The development of new antibiotics is incredibly important and we have seen the field move very slowly in recent times, but we still need to be careful with the overuse of antibiotics. Even if bacteria do not become resistant to this antibiotic, the same issues we’ve discussed pertaining to the overuse of antibiotics still exist. This antibiotic seems to be quite powerful and ridding our guts of bacteria on a regular basis can cause increased levels of obesity in children among countless other public health problems. It is important that just because an antibiotic does not cause resistance, we do not overuse it.
We look forward to the further developments with teixobactin and hope to see this move to clinical trials in the near future. This new antibiotic has only been tested so far in mice and will need to be tested further in animals and later humans. The authors estimate that if all goes well, this new antibiotic could be on the market in about 4 or 5 years (they hope to be in clinical trials in two years with clinical trials taking an additional two to three years).