Common example of fungi hyphae
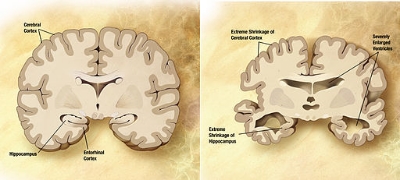
Alzheimer’s disease is a brain disease in which slow and irreversible neuronal deterioration occurs. It is characterized by the accumulation and aggregation of proteins in the brain and central nervous system (CNS), although no one knows the cause of this protein aggregation, or if these amyloids are even responsible for the neurodegeneration that occurs, rather than just associated with it. More recently, some scientists believe that Alzheimer’s is a disease caused by inflammation, because sufferers of the disease have high levels of many inflammatory signals in their brains. Indeed, some infections that would drive inflammation have been found in Alzheimer’s patients, but nothing convincing as of yet. This week though, scientists from Spain discovered that a fungal infection in the brain is highly associated with the disease. They published their results in Nature Scientific Reports.
The scientists made histological sections from the brains of 10 patients with Alzheimer’s and 10 healthy controls, and stained them for the presence of fungi. Remarkably, all 10 of the patients with Alzheimer’s showed signs of various fungi, whereas none of the healthy controls did. The fungi were seen both intracellularly and extracellularly, meaning that in some cases the fungi actually entered the neurons in the brain. The fungi included both yeasts, such as Sachromyces cerevisae, as well hyphae forming fungi such as Neosartorya hiratsukae. In addition, the scientists found traces of these fungi in the blood of the Alzheimer’s patients as well, suggesting that they may originate through common pathways, and spread into the brain.
While this study does not in any way prove these fungi are causing the disease, it certainly is compelling data that they are primary culprit for the disease. As the authors state, if one were to assume that the etiology of the disease is caused by the fungi, all the symptoms of the disease can be explained. For example, the slow progression and inflammatory nature of the disease. Fortunately, If the fungi are responsible there could be many possible therapeutic approaches, including antifungals.