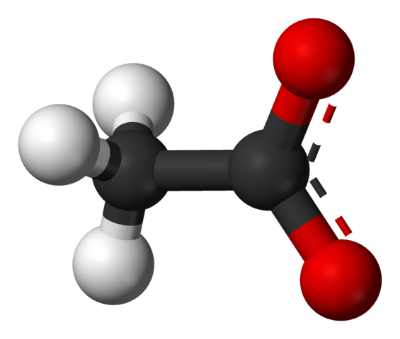
Ball and stick representation of an acetate molecule, CH3COO-
Hirschsprung disease is a disorder in which a baby is born without nerves in part or all of the large intestines, rendering them functionless. Hirschsprung-associated enterocolitis (HAEC) is a complication of Hirschsprung disease (HD), in which the intestines become inflamed due to infection. HAEC is a common cause of death in children with Hirschsprung disease, but the real cause of infection in not very well understood yet. Poor immunity, poor intestinal wall function, and an altered gut microbiome are thought to contribute to the issue. An important role of the gut microbiome is to produce short chain fatty acids (SCFAs) from complex and indigestible fiber. The short chain fatty acids contribute to bacterial homeostasis of the gut, and so they may be associated with intestinal issues observed in HAEC. Scientists from California, Michigan, and Sweden set out to test this possible connection by measuring the SCFA, and SCFA-producing bacterial composition in HD children who have HAEC. The study was published by the Journal of Pediatric Surgery.
The study population consisted of 18 children with HD, with ages ranging from 3 months to 8 years, and a median age of 2.7 years. Nine participants had a history of HAEC, while nine did not. Fecal samples were collected from the children and analyzed for SCFAs and bacterial composition. Among the children involved in the study, there were no significant differences in early feeding type, probiotic use, complications unrelated to HAEC, and length of HD diagnosis. One patient in the HD group and two in the HAEC group had trisomy 21, better known as Down Syndrome.
Total fecal SCFA composition in children with a history of HAEC was four-fold lower than that of HD patients who did not have a history of HAEC. When broken into individual SCFAs, the children with HAEC had substantially less acetate in their stools, but actually slightly higher butyrate levels compared to non-HAEC. Interestingly, the HAEC patients actually had higher levels of butyrate and acetate producing bacteria, despite the dramatically lower acetate levels. The authors suggest that perhaps the butyrate producing bacteria are actually converting acetate to butyrate, resulting in higher levels of both butyrate and butyrate producing bacteria, along with lower levels of acetate.
While we still don’t know a cause for Hirschsprung-associated enterocolitis, this study does provide an association between HAEC episodes and alteration of short chain fatty acid composition of the large intestines. This study is limited by its small sample size and other factors that are difficult to account for, but the results still do help scientists identify possible causes of the disease.