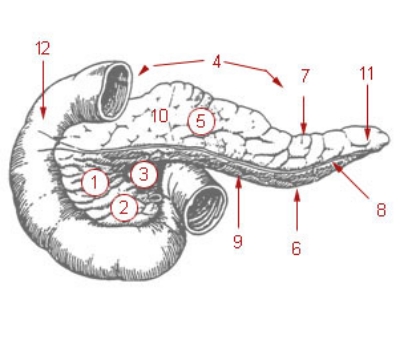
The pancreas. 1: Head of pancreas 2: Uncinate process of pancreas 3: Pancreatic notch 4: Body of pancreas 5: Anterior surface of pancreas 6: Inferior surface of pancreas 7: Superior margin of pancreas 8: Anterior margin of pancreas 9: Inferior margin of pancreas 10: Omental tuber 11: Tail of pancreas 12: Duodenum
Acute pancreatitis is a sudden and severe inflammation of the pancreas. It is responsible for many emergency room visits each year, but what causes its onset is unknown. Most cases are mild, and can be treated with very passive measures, such as fasting or rehydration. Other cases though (around 25%), are more severe, and require medical interventions, such as surgery. Recently, researchers in China conducted a clinical trial on people with acute pancreatitis in order to figure out what, if any, connections existed between the microbiome this disease. They published their results in the journal Pancreas.
The researchers sampled the feces and blood of 76 patients with acute pancreatitis every few days as the disease progressed (44 were severe cases and 32 were mild), along with 32 healthy controls. They discovered a dramatic decrease in microbiome diversity occurred in those people with pancreatitis, which was characterized by an increase in Enterococcus and a decrease in bifidobacteria compared to controls. In addition, pro-inflammatory molecules in the blood were directly correlated with the abundance of Enterococcus in these patients.
It is difficult to connect the microbiome to many inflammatory diseases because the mechanisms for how this occurs are still not totally understood. Hence, many studies, like this one, are only able to show a correlation between the microbiome and these diseases. Still though, these correlations can be powerful, and at the very least show the need for more research. So while it may not be true that a dysbiosis causes acute pancreatitis, they are clearly associated.